Pelvic pain is a common symptom and reason for women to request medical evaluation. Many times, the pain is mild and temporary. The cause of the pelvic pain may never be explained. There are many different causes of pelvic pain since so many organ systems are normally found in the pelvis. Sometimes, the pain is significant, whether in the severity or frequency of the pain. If the pain interferes with the woman’s quality of life, then it is time for further evaluation and information.
Sudden onset of pelvic pain (acute pelvic pain) may lead women to seek emergency evaluation. Acute pelvic pain may be caused by inflammation from an infection. Trauma is another possible cause. Acute pelvic pain is rarely a result of a situation in which the normal circulation of blood is decreased or stopped to a pelvic organ. Twisting of the blood supply to the ovary (ovarian torsion) may be infrequently diagnosed.
Pelvic pain for most women develops and is observed by her as an unpleasant trend that impacts her normal lifestyle. Chronic pelvic pain is diagnosed if the symptom has been a problem for at least 6 months.
Evaluation
The woman may start the assessment with her primary care office, seek out a specialist, or even go to the emergency room. Not every episode of pelvic pain needs to be evaluated in an emergency setting.
1. History
There are often coincidental symptoms with the pelvic pain that can help with the diagnosis. Many women experience gynecologic reasons for pelvic pain. The healthcare provider may ask about the timing of the pain in relation to the woman’s menstrual cycle. Are there activities that cause or worsen the pelvic pain? When the pain occurs, is it in the same area of the body? Other questions that may suggest a gynecologic cause include presence of vaginal discharge, pain with intercourse (known as dyspareunia), and previous gynecologic surgery or family history of female-related problems.
Gastrointestinal causes are also common reasons for pelvic pain. Symptoms including nausea, vomiting, bowel habit changes, or fever may be linked to pelvic pain. History of gastrointestinal problems and conditions in the woman or family are also important to report.
Urologic sources of pelvic pain are common in women. Painful urination, change in the appearance of the urine or urinary frequency may suggest the connection of pelvic pain to the urinary tract. A history of urinary problems is valuable to report to the healthcare provider.
General medical information will add to the assessment. Past medical history includes previous surgery, medical conditions, and treatments. Family history can be helpful since some causes of pelvic pain are known to run within female family members. Pregnancy history including any delivery details and problems can play a role in the diagnosis of the woman’s pelvic pain.
2. Physical exam
Various aspects of an exam will be important to make a diagnosis and provide the best recommendations. If pelvic pain is the problem, then an exam of the abdomen and pelvis is needed. Medical care trends include the promotion of telemedicine to treat problems without the patient’s inconvenience of a personal visit and exam.
Hopefully, many women are accurately evaluated and treated if they use this service with desirable outcomes. Recurrent or persistent pelvic pain without improvement should be evaluated by a hands-on physical exam. Some medical information is not possible to learn without a provider performing a thorough and adequate physical exam of the abdomen and pelvis.
3. Labs
Some blood work or lab tests may shed some light on the cause of pelvic pain. The blood tests may include a complete blood count to evaluate for anemia and infection, liver, and kidney function. Urinalysis, possibly with culture and sensitivity, is helpful.
Pelvic pain can be caused by infections from some sexually transmitted diseases. Therefore, some tests may be recommended to eliminate the possible cause. This evaluation is performed with samples from blood, vagina, or urine.
4. Imaging
The most common evaluation is by an ultrasound of the pelvis. A transvaginal ultrasound can provide some valuable information about the pelvic organs. Normal anatomy is considered in comparison to what is observed. Any abnormality of size, shape or position is noted.
CT (computerized tomography) scans are another common imaging method. These scans are usually available in hospitals and specialized imaging centers. Gynecologic evaluation usually starts with ultrasound. CT imaging may be ordered for gastrointestinal or urologic assessment.
5. Surgical evaluation
There may be situations in which a surgical assessment is indicated for pelvic pain, especially if all other results are normal or inconclusive. Some conditions, such as endometriosis, are only diagnosed through surgery. Diagnostic laparoscopy is a minimally invasive outpatient surgery to visualize the pelvis. In most cases, conservative surgical treatment at the time of diagnosis is possible.
If abnormal vaginal bleeding has coincided with the pelvic pain, other conservative outpatient procedures may be offered as hysteroscopy with dilatation and curettage (D&C) of the uterus. An endometrial polyp is an example of the anatomic finding that might cause pain with bleeding. Again, the surgeon will likely remove any abnormal appearing tissue with the hope to improve symptoms.
Causes
There are many sources of pelvic pain in women. The following list is not comprehensive but may serve as a guide. Related symptoms can indicate a possible cause.
1. Gynecology
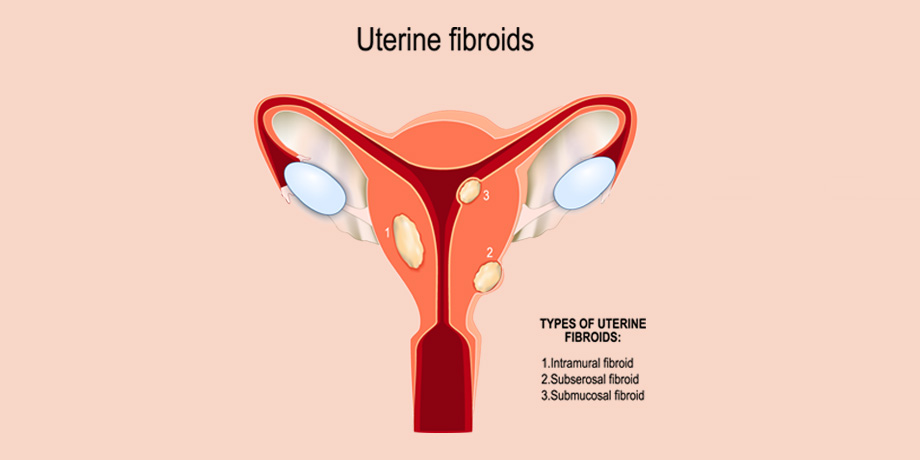
There are various anatomic abnormalities as uterine fibroids and ovarian enlargement due to abnormal ovarian cysts or masses that may be discovered with a pelvic exam or ultrasound. Over half of women with persistent pelvic pain will have endometriosis, so diagnostic surgical evaluation and possible surgical treatment is necessary. Some infections may cause pelvic pain. Sexually transmitted diseases as chlamydia may cause inflammation and pain. Specific medical treatment would be needed in these cases.
2. Gastroenterology
The digestive tract shares space in the pelvis with the female pelvic organs. Pelvic pain and bloating may be a result of other problems than those specific to women. Symptoms as diarrhea, constipation, or bleeding with bowel movements suggest non-gynecologic problems. A more serious cause of acute pelvic pain is appendicitis. A gastrointestinal consultation could be needed.
3. Urology
In a similar way, the urinary tract also shares the pelvis with the female anatomy and the digestive tract. Pelvic pain can be a result of a urinary tract infection. Other urologic causes of pelvic pain may include kidney/bladder stones and bladder inflammation (interstitial cystitis).
4. Other causes
Accidental trauma from exercise, from a fall or lifting heavy objects could lead to unexpected pelvic pain. Abuse (sexual, physical, emotional) may result in pelvic pain, whether from tissue injury or psychologic injury.
Treatment
If there is a reasonable possibility that the pelvic pain is caused by a gynecologic problem, medical management is often the first line of therapy. Anti-inflammatory medication or analgesics (for example, acetaminophen) may improve pain symptoms. Hormonal therapy using low dose combination therapy as birth control pills or progesterone only therapy may improve symptoms of pelvic pain.
Again, there are surgical treatments that may be helpful. No gynecology provider should ever offer extreme treatments as removing organs as the uterus (hysterectomy) or ovaries (oophorectomy) without proper evaluation and discussion of the medical facts.
Summary
Pelvic pain is a concern if it has lasted for many months, is worsening, or interfering with normal life. A woman experiencing such pelvic pain should seek the help of her trusted women’s health provider to get the evaluation and possible treatment that she may need.